Researchers find how pathogenic bacteria trigger Crohn's disease
The findings of a recent study headed by Weill Cornell Medicine and NewYork-Presbyterian researchers, suggests that changes in a single gene allow dangerous gut bacteria to trigger the inflammation that underlies Crohn's disease.
- Country:
- United States
The findings of a recent study headed by Weill Cornell Medicine and NewYork-Presbyterian researchers, suggests that changes in a single gene allow dangerous gut bacteria to trigger the inflammation that underlies Crohn's disease. One day, these discoveries might make it easier for medical professionals to choose more precise treatments for people with immunological disorders.
This specific host gene, AGR2, encodes a component of the cell's machinery that aids in appropriately preparing new proteins so they can aid in warding off "bad" bacteria. The cell is stressed when a process is disrupted by anything from microorganisms to inflammatory circumstances. Extremes in AGR2 expression--when it is either overly active or completely silent--are linked to such stress and the cell's response to it, and they served as the inspiration for the study detailed in Cell Reports. The investigators already suspected the cell's stress response plays a central role in the development of Crohn's. In addition to AGR2, many other variants linked to Crohn's are involved in this response, according to co-senior author Dr Randy Longman, associate professor of medicine in the Division of Gastroenterology and Hepatology and the director of the Jill Roberts Center for Inflammatory Bowel Disease at Weill Cornell Medicine and NewYork-Presbyterian/Weill Cornell Medical Center.
"What makes this study unique is that we discovered a link between one of these stress-related genetic susceptibilities and changes in the gut microbial community leading to the development of this disease," he said. The lining of the gut, primarily in the small intestine and colon, is damaged by chronic inflammation in more than half a million Americans who have Crohn's disease, a type of inflammatory bowel disease (IBD). It can be caused by a hazy concoction of elements, including genetic vulnerability and the presence of specific microorganisms.
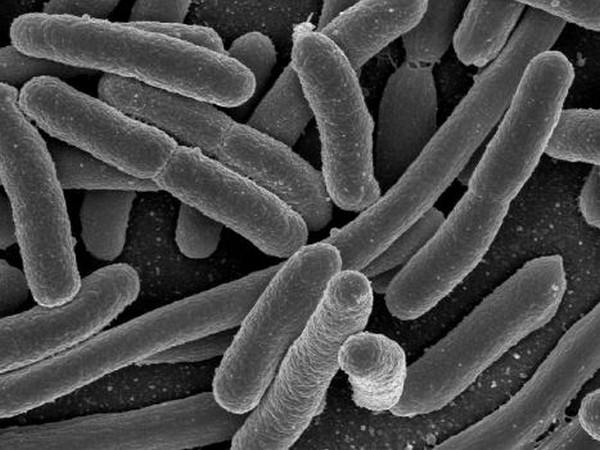
When co-senior author Dr Steven Lipkin, vice chair for research at Weill Cornell Medicine's Weill Department of Medicine, and a medical geneticist at New York-Presbyterian/Weill Cornell Medical Center, genetically modified mice to prevent expression of the AGR2 gene for a different project, they unexpectedly developed inflammation similar to Crohn's disease. He and his collaborators linked that inflammation to microbes known as adherent-invasive Escherichia coli (AIEC), which are among the bacteria implicated in Crohn's.
"My lab began studying AGR2 more than 10 years ago. Now, there are more than 400 publications about the gene," said Dr Lipkin, who is also the leader of the Cancer Genetics and Epigenetics Program at the Sandra and Edward Meyer Cancer Center at Weill Cornell Medicine. "This gene drives an important pathway relevant for IBD, cancer metastasis and other clinically relevant pathways, and is a promising precision medicine therapy target and co-theragnostic." Theragnostics are treatment strategies that combine diagnostics and therapies. Dr Longman, who investigates these bacteria and their function in Crohn's illness, was subsequently approached by Dr Lipkin. Together, they established a link between changes in AGR2 activity levels and increases in the class of bacteria that AIEC belonged to, together with a collaborative team that also included Dr Kenneth Simpson at Cornell's Ithaca campus and Dr. Balfour Sartor at UNC. Then, using mouse tests, scientists proved that the inflammation is brought on by both AIEC and an aberrant stress response. Furthermore, their findings suggested that a changed reaction promotes the growth of AIEC, reinforcing the disease.
The researchers continued to identify the inflammatory process that was sparked by this encounter. Their research found a connection between it and the generation of the immunological signal IL-23, which is known to contribute to Crohn's disease. "IL-23 is an important driver of IBD and colorectal cancer tumorigenesis and an important therapeutic target," Dr Lipkin said. "Our research has the potential to bring precision medicine to IBD and develop anti-metastasis cancer therapies for patients."
Doctors currently have numerous ways to treat Crohn's, including some that target specific aspects of its complex biology. However, they have little guidance on which treatment to use for a given patient. By connecting AGR2 and AIEC with IL-23, this study provides the sort of context that could help to direct these decisions, according to Dr Longman. (ANI)
(This story has not been edited by Devdiscourse staff and is auto-generated from a syndicated feed.)
- READ MORE ON:
- Americans
- Cell Reports
- Crohn
- Escherichia
ALSO READ
Noida: 12 held from fake call centre for duping Americans
Americans think a president's power should be checked, AP-NORC poll finds — unless their side wins
Loneliness can kill, and new research shows middle-aged Americans are particularly vulnerable
Biden seeks to cancel some interest on student loans, aiding 23 million Americans
US considers easing warnings for Americans traveling to China










