Rwanda’s Response to First Marburg Virus Outbreak Sets New Regional Benchmark
After investigating a cluster of unexplained illnesses and deaths in Kigali, Rwanda's Ministry of Health officially declared the outbreak on 27 September 2024.
- Country:
- Rwanda
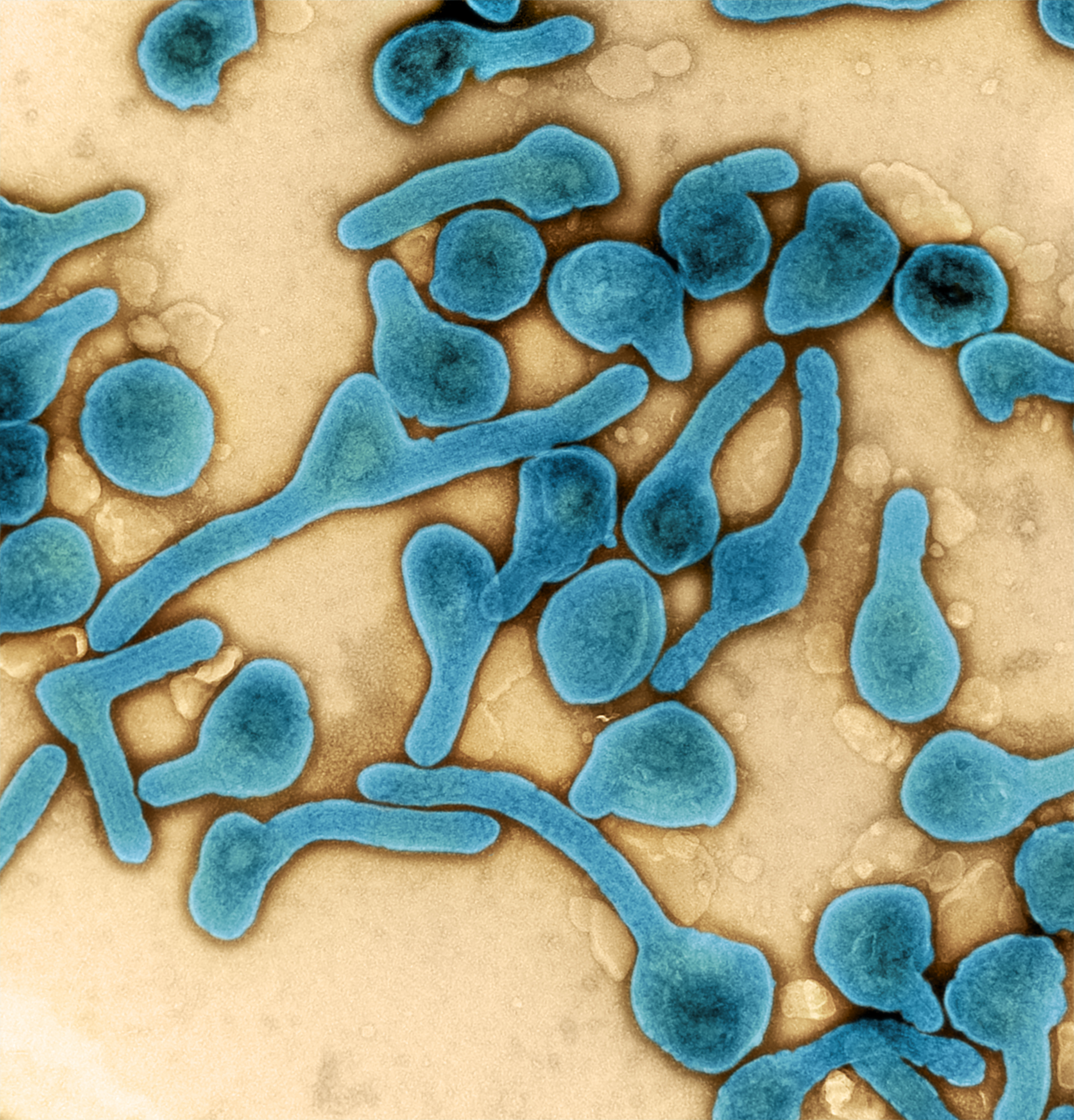
In September 2024, Rwanda faced an unprecedented public health crisis: its first-ever outbreak of a filovirus—Marburg Virus Disease (MVD). This severe and often fatal illness, with a case fatality rate historically ranging from 24% to 88%, struck suddenly and posed a significant threat to national health security. After investigating a cluster of unexplained illnesses and deaths in Kigali, Rwanda's Ministry of Health officially declared the outbreak on 27 September 2024.
The virus, known for causing hemorrhagic fever with devastating outcomes, quickly overwhelmed parts of the healthcare system. Particularly alarming was the infection of healthcare workers, revealing vulnerabilities in infection prevention and control (IPC) practices across healthcare settings. This underscored the urgency for an immediate, organized, and multisectoral response.
Rapid, Unified Response Through Strategic Partnerships
Spearheaded by Rwanda’s Ministry of Health, the response was nothing short of remarkable. Thanks to the swift collaboration of local and international partners, Rwanda managed to initiate a coordinated emergency action plan within days of the outbreak confirmation.
Key partners included:
-
World Health Organization (WHO)
-
European Union Humanitarian Aid (ECHO)
-
UK Foreign, Commonwealth and Development Office (FCDO)
-
Various other development and humanitarian organizations.
Through their support, critical resources were mobilized:
-
Deployment of teams of technical experts.
-
Rapid procurement and distribution of personal protective equipment (PPE), laboratory testing kits, and case management tools.
-
Accelerated training and capacity building for healthcare workers at all levels.
WHO’s immediate technical and operational assistance proved vital, providing direct support for outbreak coordination, surveillance strengthening, laboratory operations, and strategic risk communication.
Dr. Brian Chirombo, WHO Representative to Rwanda, emphasized, “The generous funding from ECHO and FCDO, among others, was instrumental in ensuring the availability of essential supplies and empowering health workers during a critical time. This support enabled swift laboratory testing, enhanced protection for healthcare workers, and the delivery of quality patient care, ultimately resulting in improved health outcomes.”
Deployment of Regional Expertise
Recognizing the need for reinforced technical capacity, Rwanda’s Ministry of Health requested assistance from WHO, leading to the rapid mobilization of a diverse group of international experts. Areas of specialization included:
-
Coordination and outbreak management
-
Surveillance and contact tracing
-
Laboratory testing and diagnostics
-
Clinical case management
-
Infection prevention and control (IPC)
-
Mental health and psychosocial support (MHPSS)
-
Logistics and risk communication/community engagement (RCCE)
Importantly, 39 seasoned health professionals from Liberia, Sierra Leone, and Uganda were deployed through WHO’s AVoHC-SURGE program. Having first-hand experience in managing previous filovirus outbreaks, these experts provided invaluable support, addressing human resource shortages caused by the early infection of Rwandan healthcare workers.
This South-to-South collaboration model—where neighboring African nations support each other—proved critical. Shared cultural understanding, language familiarity, and regional solidarity enhanced the effectiveness and appropriateness of the response, offering a strong model for emergency preparedness across the continent.
Strengthening Healthcare Capacity Through Training
One of the pillars of Rwanda’s success was the rapid and comprehensive upskilling of its healthcare workforce. With technical support from WHO and funding from ECHO and FCDO:
-
Extensive trainings were conducted across the health system, including specialized hospitals, district hospitals, community health centers, and Points of Entry (POEs).
-
Healthcare workers were trained in early detection, safe patient handling, case management protocols, and best IPC practices.
-
Updated national guidelines and standard operating procedures (SOPs) were swiftly developed and disseminated.
-
Emphasis was placed on community engagement, empowering local populations with accurate information to counter misinformation and stigma.
This capacity-building effort not only addressed the immediate needs of the outbreak but also strengthened Rwanda’s long-term resilience against future epidemics.
Achieving a Historic Milestone: Lowest Fatality Rate
Thanks to coordinated efforts and effective containment strategies, Rwanda achieved a case fatality rate of 22.7%—the lowest recorded among Marburg Virus Disease outbreaks in Africa.
This achievement is significant considering the deadly nature of the Marburg virus and the historical difficulties other countries have faced in controlling such outbreaks. Rwanda’s success demonstrates the tangible impact of investing in preparedness, quick mobilization, and strategic partnership building.
Lessons for the Future
The Marburg outbreak response in Rwanda illustrates several critical lessons for global health security:
-
Strategic partnerships and cross-border collaboration are essential.
-
Rapid resource mobilization and expert deployment can dramatically alter the course of an outbreak.
-
Healthcare system strengthening at all levels must remain a top priority.
-
Community involvement and trust-building are key to successful outbreak containment.
The efforts in Rwanda will likely serve as a model for regional and global health emergency responses, emphasizing that preparedness, swift action, and strategic coordination are non-negotiable elements in mitigating future infectious disease threats.
Rwanda’s response to its first Marburg Virus Disease outbreak stands as a monumental public health achievement. It showcases the power of resilience, partnerships, and rapid action, while reinforcing the necessity for continuous investment in health system strengthening and emergency preparedness.
As the world faces evolving health threats, Rwanda’s experience serves as both inspiration and a blueprint for future collaborative action across Africa and beyond.
ALSO READ
Health Headlines: Significant Developments in Drug Approvals and Public Health Policies
Indore's Public Health Crisis: Swift Government Action
Water contamination in Indore: CM orders suspension of additional municipal commissioner, Public Health Engineering official.
Union Health Minister Pushes for Enhanced Public Healthcare Initiatives
NZ Pays Tribute to Dame Karen Poutasi’s Lifelong Service to Public Health










