No vaccine? No problem: AI generates targeted antibodies against VEEV
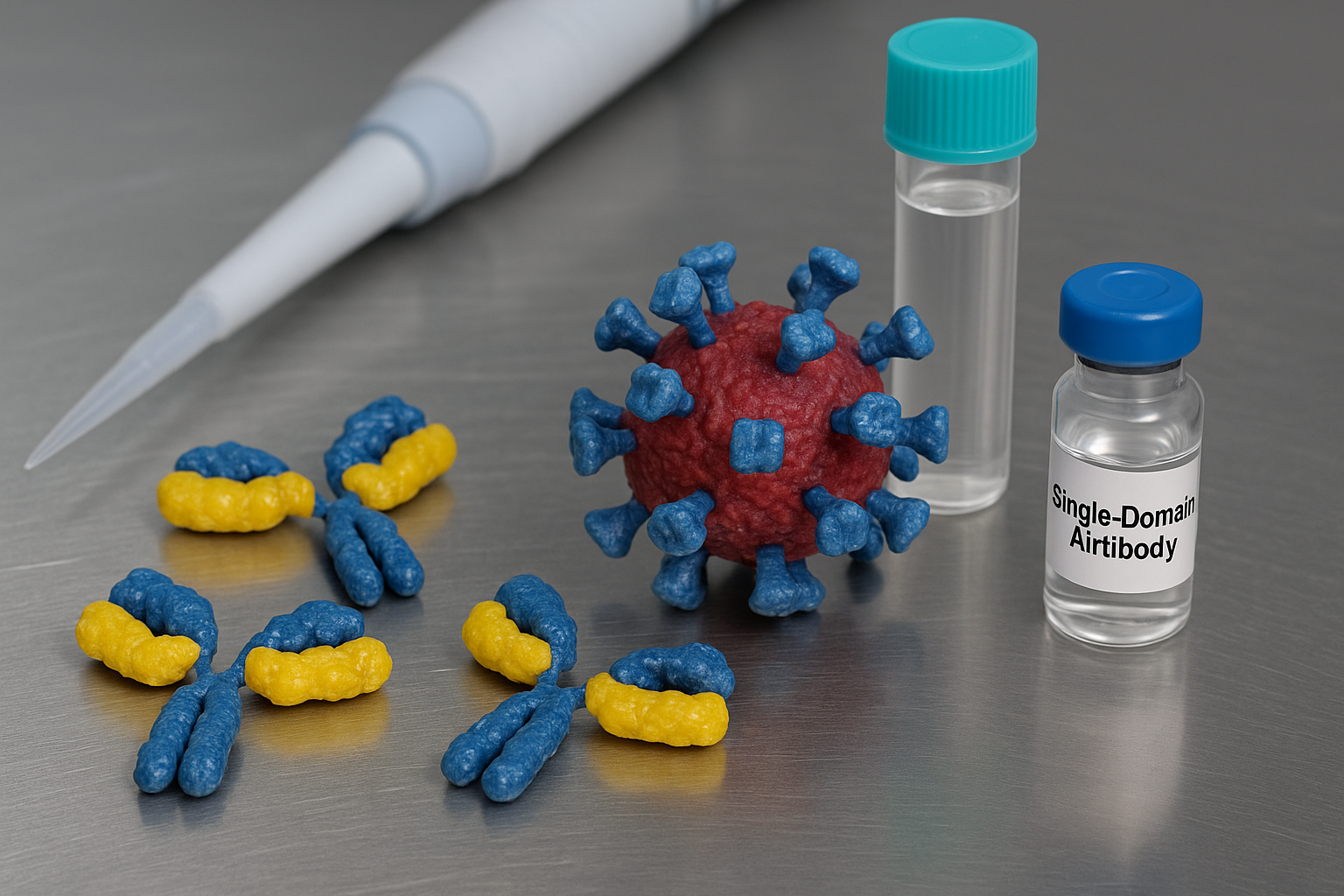
The study demonstrates how generative deep learning, when combined with structural prediction and affinity modeling, can swiftly produce viable therapeutic antibody candidates. Leveraging ProtGPT2, a 738-million parameter protein language model, researchers fine-tuned the algorithm with a curated dataset of 245 single-domain antibody (sdAb) sequences, including 62 VEEV- and CHIKV-binding antibodies and 183 against SARS-CoV-2. This training allowed the model to learn critical sequence patterns associated with viral neutralization.
Researchers have turned to generative artificial intelligence to accelerate the development of next-generation therapeutics. Venezuelan equine encephalitis virus (VEEV), a mosquito-borne alphavirus known for its neurological impacts and aerosol transmissibility, remains a critical biothreat with no FDA-approved vaccine or targeted therapy currently available.
In a landmark study published in Antibodies, titled “Generative Deep Learning Design of Single-Domain Antibodies Against Venezuelan Equine Encephalitis Virus,” scientists from the U.S. Naval Research Laboratory and the Naval Research Enterprise Internship Program unveiled a rapid AI-driven framework for engineering VEEV-neutralizing nanobodies, offering a potentially transformative advance in biodefense and antiviral drug development.
How does AI transform the antibody discovery pipeline?
The study demonstrates how generative deep learning, when combined with structural prediction and affinity modeling, can swiftly produce viable therapeutic antibody candidates. Leveraging ProtGPT2, a 738-million parameter protein language model, researchers fine-tuned the algorithm with a curated dataset of 245 single-domain antibody (sdAb) sequences, including 62 VEEV- and CHIKV-binding antibodies and 183 against SARS-CoV-2. This training allowed the model to learn critical sequence patterns associated with viral neutralization.
The team generated over 44,000 novel sequences through an optimized inference process, narrowing the pool down to 250 candidates based on amino acid frequency distribution, solubility metrics, and structural realism. Each top sequence was paired with the VEEV E2 glycoprotein using AlphaFold2-multimer to predict binding conformations and interaction stability. The resulting complexes were evaluated using the Prodigy algorithm to estimate dissociation constants, filtering down to 41 high-affinity candidates.
Further screening using Ramachandran plots, physiochemical profiles, and BLAST comparisons reduced the final shortlist to eight unique sdAbs that exhibited optimal structural integrity and novelty. These sdAbs were unlike any previously cataloged antibodies in GenBank or the SAbDab database, with distinct complementarity-determining regions (CDRs) critical for antigen recognition.
Can AI-engineered sdAbs neutralize VEEV in practice?
To test real-world potential, the final eight sdAbs were expressed in Escherichia coli using engineered pET22b plasmids with solubility-enhancing DDDDK tags. Protein production was successful for six sdAbs, which then underwent enzyme-linked immunosorbent assays (ELISAs) against irradiated TC-83, a biosafety-level-2 strain of VEEV. Four candidates (a155, a16, a18, a19) demonstrated antigen binding, with a155 and a18 showing the strongest responses.
These two top candidates were then subjected to plaque reduction neutralization tests (PRNT) using Vero cells. A155 and a18 successfully reduced viral plaques by 50% at concentrations of 44 and 39 µg/mL, respectively—comparable to known llama-derived sdAbs like V2B3, albeit weaker in overall potency. These outcomes validated the in silico predictions, confirming real-world neutralization potential and suggesting that AI-designed sdAbs could offer protective efficacy under laboratory conditions.
The study also examined protein–protein interfaces using AlphaFold2-multimer to predict epitope contacts. Both a155 and a18 showed high interaction density, 142 and 135 contacts respectively, primarily mediated by CDR3 loops. These findings correlated with their superior ELISA and PRNT outcomes. Comparative structural modeling further indicated that these sdAbs target similar epitopes to known neutralizers, such as residue K222 and Q225 on E2, which are essential for viral attachment and entry.
What are the broader implications for AI in viral defense?
While the AI-designed sdAbs demonstrated moderate neutralization, the significance of this research lies in the speed and adaptability of the generative approach. From model fine-tuning to candidate selection and validation, the entire process was condensed to approximately 24 hours using a single consumer-grade GPU. In contrast, traditional antibody discovery through immunization and phage display can take weeks or months.
The study acknowledges limitations, including the relatively low predictive accuracy (~30%) of AlphaFold2-multimer for antibody–antigen interfaces and the limited dataset available for VEEV. Nevertheless, the authors point to imminent advancements such as AlphaFold3 and more powerful generative models like ESM3 and Boltz-1 that could significantly enhance precision and solubility predictions.
Importantly, the researchers emphasize that generative models are not replacements for conventional discovery but are complementary tools that can dramatically shorten response times during outbreaks or bioterror events. The framework also provides a repeatable method for tackling other alphaviruses or understudied pathogens lacking rich datasets. Solubility remains a production challenge, with two of the eight candidate sdAbs proving insoluble despite pI modifications. However, newer tools like MPNNsol may resolve these bottlenecks in future iterations.
- FIRST PUBLISHED IN:
- Devdiscourse










